The Hidden Deficiencies Sabotaging Your Carb Metabolism (Part 2)
How to unf*ck your glucose metabolism with nutrition
Are we really still talking about this?
Yes - because this goofiness still exists.
And this.
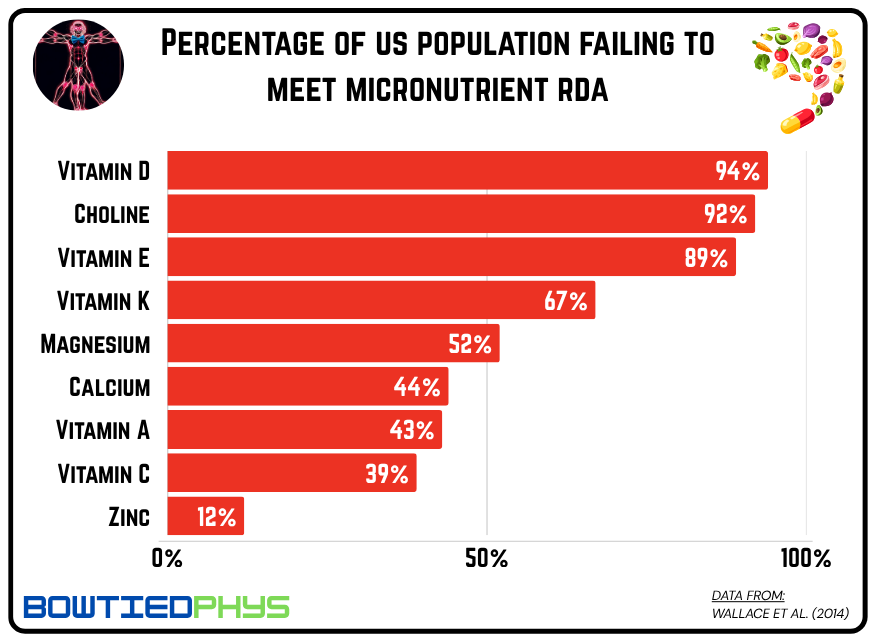
We can continue - but you get the point. Carbs aren’t the problem. But the SAD is a big part of it and if we had to summarize the sad story of the SAD (Standard American Diet) in three words: Overfed but undernourished.
The Standard American Diet is one of excess macro-nutrition & a scarcity of micro-nutrition.
Your daily energy intake is a budget. A well-balanced one prioritizes calorie spend on micronutrient-dense foods grown in fertile soil (fruits & vegetables) or have consumed a robust diet themselves (meat, poultry, & seafood). Take the inverse - a hyperpalatable combination of high-fat, high-carb, low-micronutrient energy - and that’s the hellish landscape we’ve normalized in the current metabolic state of the US.
Last week we explored how light, timing, exercise, & environment can transform glucose metabolism.
Now it’s time to step into the nutritional deficiencies holding back your mitochondrial capacity.
Here are the 14 most critical nutritional tools for functional glucose metabolism.
Deficiency #1: Magnesium
Mechanism: If the enzyme involves energy production (ATP) in our cells, it needs magnesium to function - especially true when it comes to carb metabolism. Without sufficient intracellular magnesium stores, our insulin receptors fail to function properly leading to peripheral resistance despite normal levels of insulin.
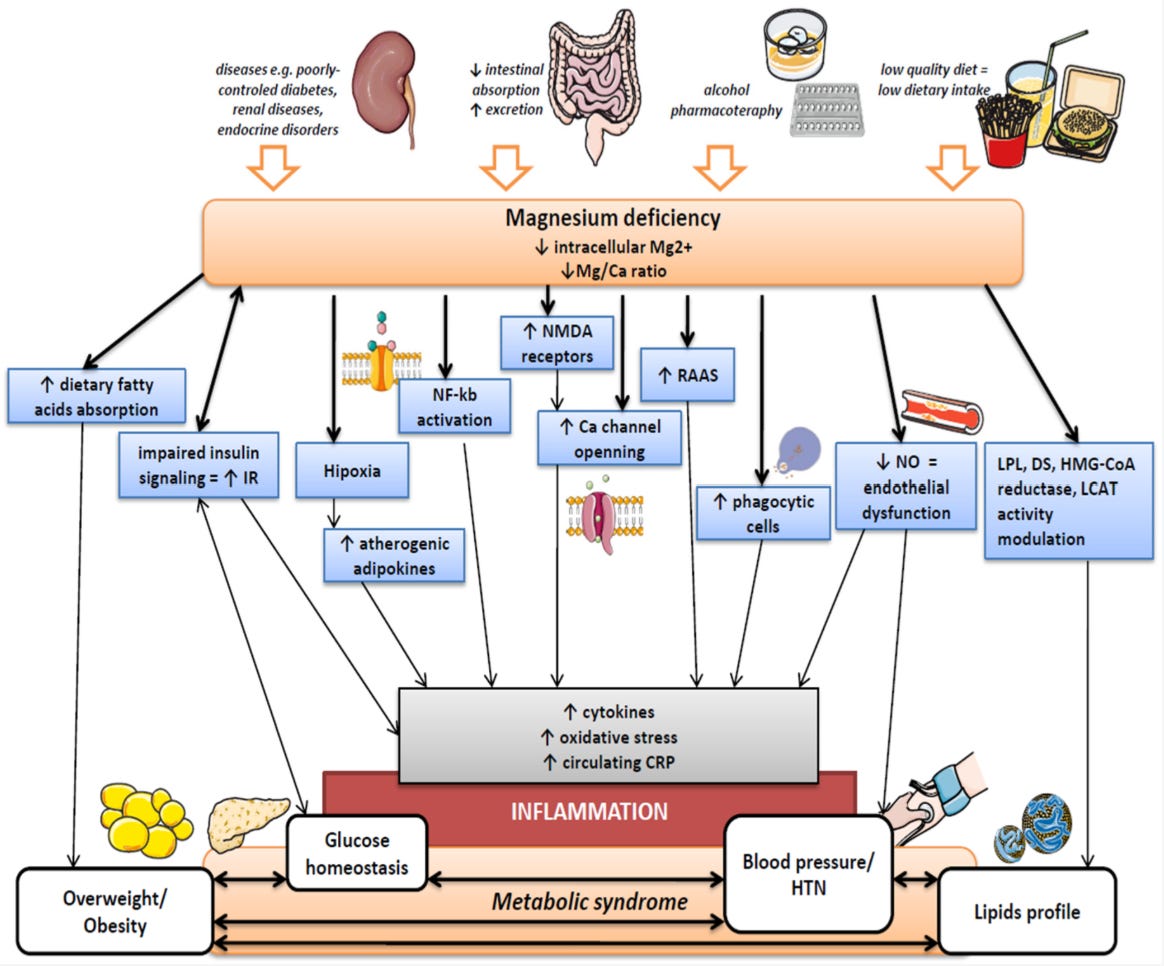
Evidence: Even in non-diabetic individuals with “normal” (*this still means deficient by the way*) magnesium levels, Guerrero-Romero et al. reported magnesium supplementation (2.5 g daily magnesium chloride) significantly improved fasting blood glucose, insulin levels & insulin sensitivity markers.
Conversely, it shouldn’t come as a surprise the likelihood of hypomagnesemia in subjects with type 2 diabetes is ~10x greater than healthy individuals.
Protocol: Achieving the optimal daily intake of magnesium is difficult through diet alone and thus why supplementation is needed. Plus our food system's mineral depletion means that even those that are dialed in nutritionally are still falling short of what we need for peak metabolic function.
Here’s how to correctly supplement one of the most critical nutrients:
Magnesium Supplementation Guide
If you’re here - chances are you’re way out in front of supplementing magnesium. But I’ve gotten tons of questions the past year regarding its practical use.
Deficiency #2: Vitamin C
Mechanism: Given vitamin C’s role as a powerful antioxidant, it makes sense we see a causal relationship between Vitamin C intake & metabolic syndrome paved via excessive levels of oxidative stress.
As crucial as vitamin C is for our redox balance state - it’s also essential for proper insulin secretion from pancreatic beta cells. When levels are low, we don’t produce the adequate insulin response to increases in blood glucose.
Evidence: Type 2 diabetics have lower vitamin C levels & higher requirements than healthy individuals needing ~150% more to maintain optimal levels. In a 2023 meta-analysis by Nosratabadi et al. across 22 RCTs & 1,500 participants, high-dose vitamin C intake ( > 1,000 mg/day) significantly improved HbA1c, fasting insulin, and fasting blood glucose in type 2 diabetics.
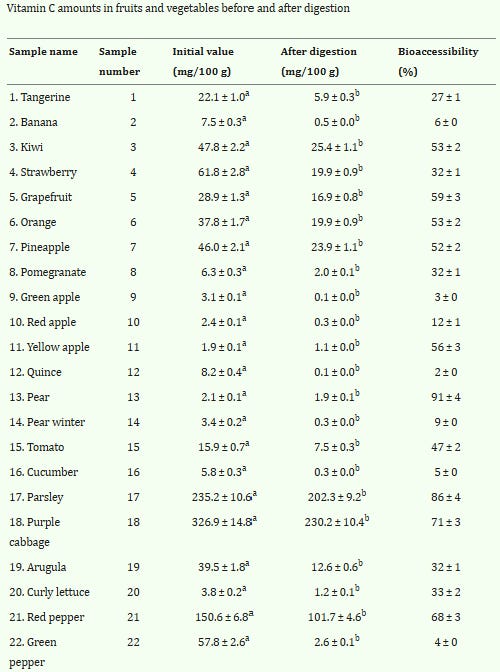
Protocol: When healthy, aim for 500 - 1,000 mg daily. If actively fighting off sickness (& gut is able to tolerate elevated doses), dose 2,000 mg every ~2-3 hrs away from meals until 8,000 - 10,000 mg is reached. Best supplemented via Acerola Powder & Liposomal Vitamin C.
Deficiency #3: Potassium
Mechanism: While high sodium intake has been the low-hanging culprit for elevated blood pressure & generally poor metabolic for decades, that long-standing narrative proved to be missing one critical element: chronic potassium deficiencies. Potassium regulates insulin release from the pancreas by maintaining proper electrical activity & supporting calcium signaling. It also supports the function of the Na⁺/K⁺-ATPase pump maintaining intracellular ionic balance and facilitating glucose uptake in muscle and adipose tissue.
Evidence: Clinical evidence supporting potassium’s role in glycemic control is robust at this point. Mild potassium deficiency reduces insulin secretion by 26% & glucose tolerance by 27%.
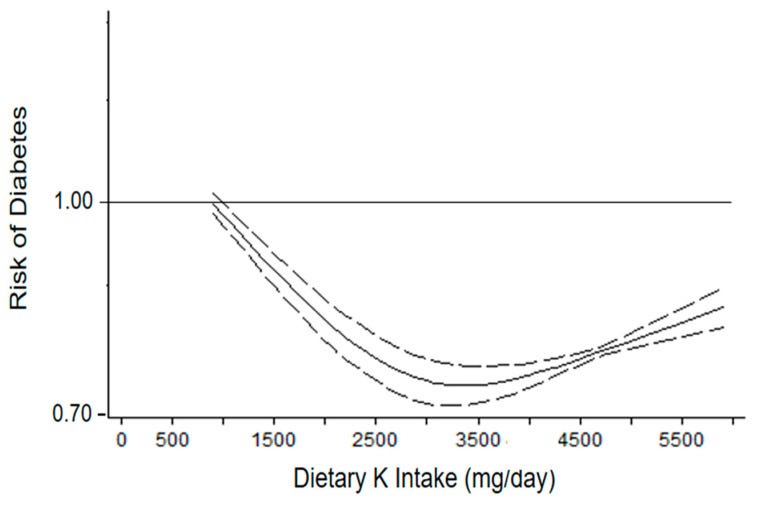
A 2022 meta-analysis across seven studies found a nonlinear relationship between dietary potassium intake and diabetes risk - protective effects were found ~3,000 mg/day.
Protocol: Even more critical than the quantity of potassium itself is the balance between two major electrolytes - potassium & sodium. Target a potassium-to-sodium ratio of ~2:1. Avoid supplementation altogether to curtail hyperkalemia risk.
Deficiency #4: Carnitine
Mechanism: Carnitine’s role as a glucose metabolism enhancer centers around its function as a cofactor for a key enzymatic process carnitine acetyltransferase (CrAT) → catalyzes the reversible formation of acetyl-carnitine from acetyl-CoA and free carnitine. When carnitine is low, fat can't enter the mitochondria efficiently for burning. This creates a backup of fatty acids in the cell interfering with insulin signaling. Thus, creating a cycle of metabolic inflexibility.
Evidence: In its supplemental form, L-carnitine is increasingly being proven as a metabolic optimization tool needed to flip the substrate switch & improve mitochondrial function. This has become increasingly clear in trials demonstrating improvements in fasting glucose levels, insulin sensitivity, & HbA1c markers.
We even see its benefits extend beyond glucose metabolism enhancements:
Protocol: If taking Acetyl-L-Carnitine (ALCAR), aim for 1,000 - 1,500 mg prior to fasted cardio. If taking, L-Carnitine Tartrate, include 2,000 - 3,000 mg into your pre-workout meal/stack.
Deficiency #5: Arginine
Mechanism: Arginine facilitates the pancreas’ ability to sense glucose & respond by producing more insulin. This happens through two main mechanisms: 1) transporting into the pancreas & creating an electrical charge triggering insulin release and 2) directly binding to and activating glucokinase → the “glucose sensing” enzyme.
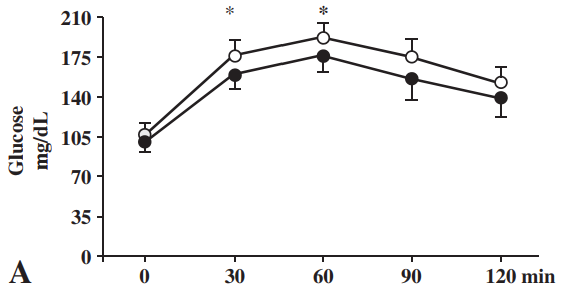
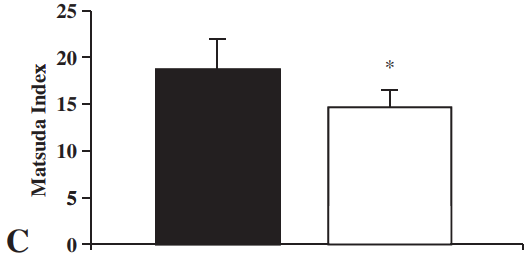
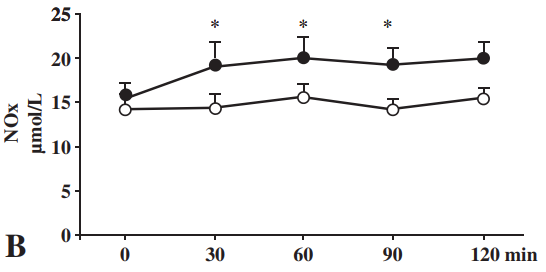
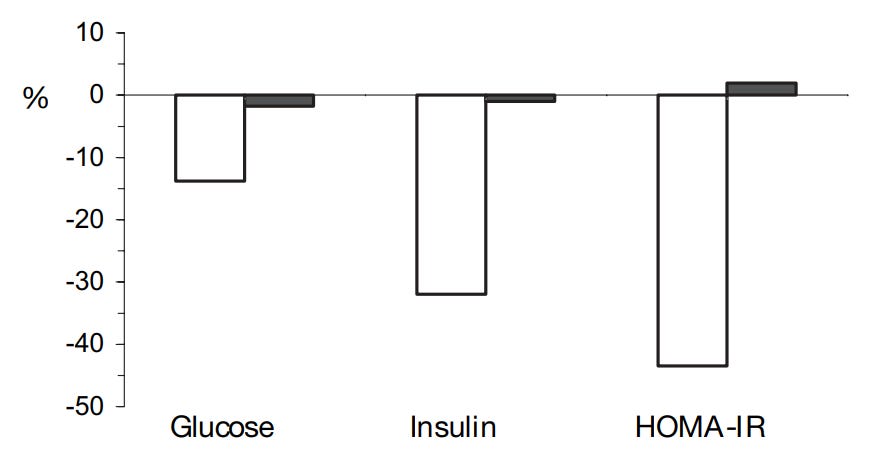
Up until today, supplementing L-arginine has shown notable improvements across a variety of glycemic biomarkers in 11 randomized controlled trials since 1997. The most notable one by Monti et al. was a 6-week crossover design trial (w/ a 12-month follow-up) supplementing 6.6 g/day of L-arginine. Some of those significant improvements included (black = L-arginine & white = placebo):
Postprandial glucose disposal
Insulin sensitivity
Nitric oxide
Protocol: 2 - 3 g/day optimal dosing obtainable from diet alone. Determined as safe up to 30 g/day for 3 months. A similar tool to boost nitric oxide output & improve resistance training pumps = L-citrulline as described in the below pre-workout post.
Deficiency #6: Glycine
Mechanism: Glycine’s impact on metabolic function can be attributed mainly to single mechanism: improved glutathione synthesis & overall antioxidant protection. It’s essential for our master antioxidant system and without adequate glycine stores, our redox balance state gets disrupted.
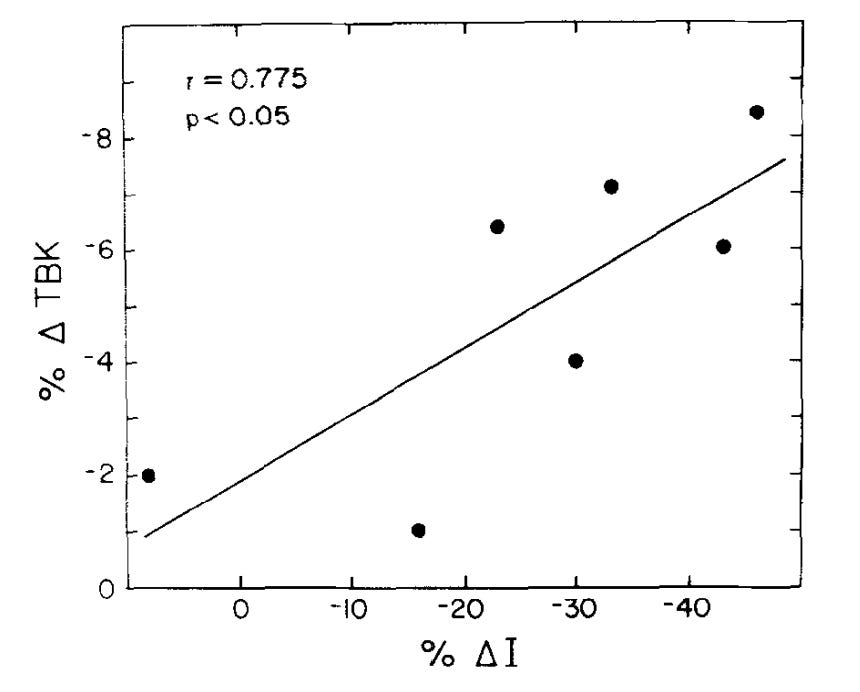
Evidence: While there exists strong association between increased glycine concentrations & the reversal of type 2 diabetes, trials regarding glycine supplementation provide even more direct evidence for its role in improving the metabolic function.
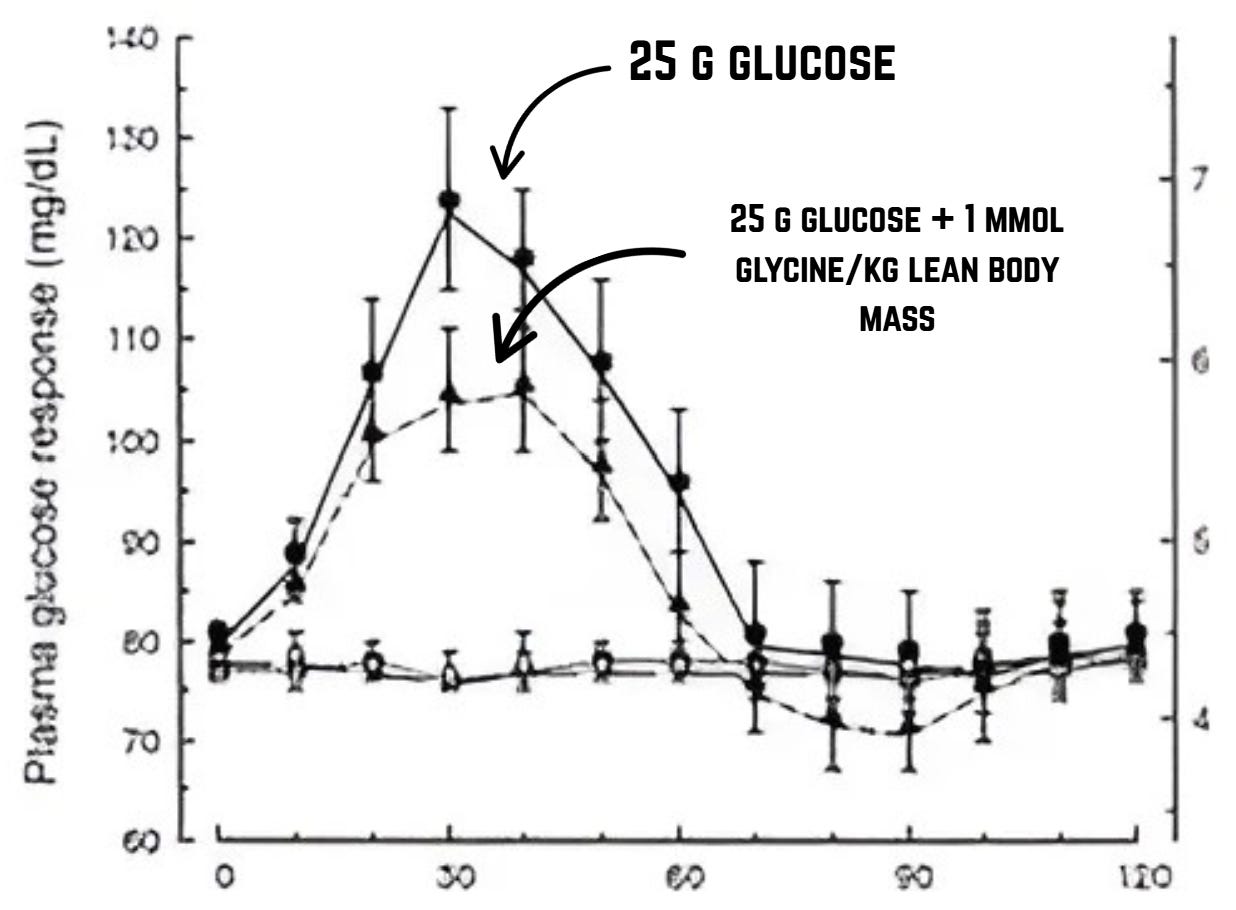
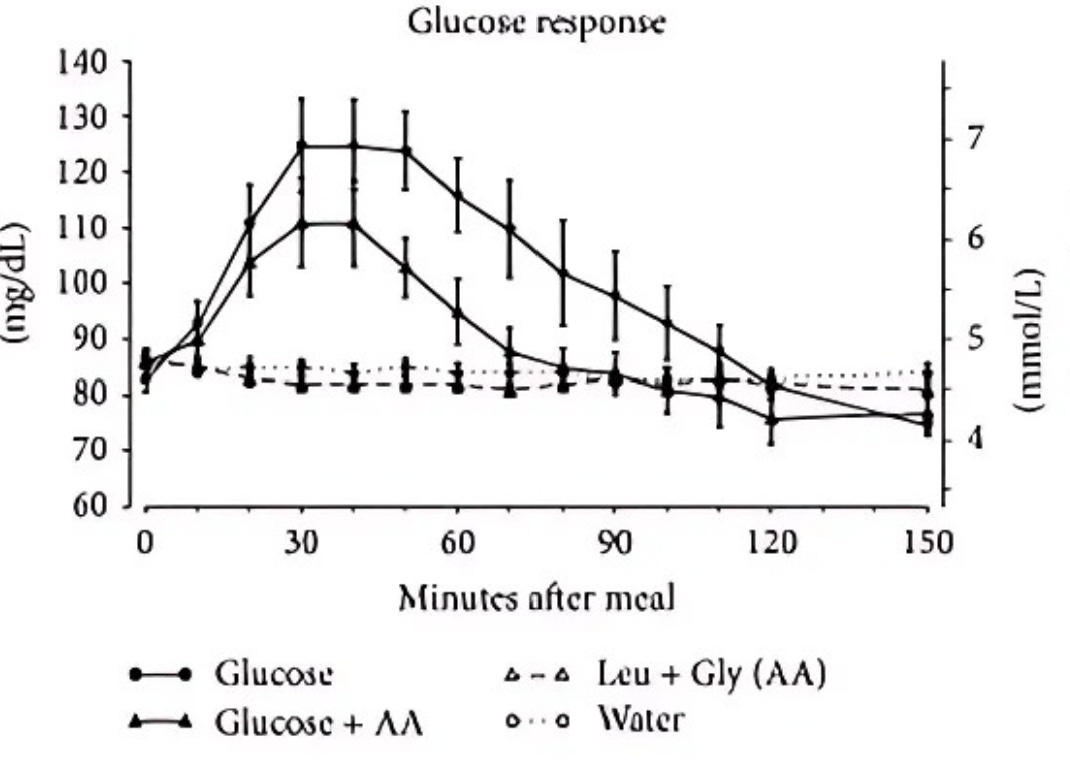
For example, Gannon et al. reported:
“When glycine was ingested with glucose, the plasma glucose area response was attenuated by > 50% compared with the response after the ingestion of glucose alone.”
Gonzalez-Ortiz et al. also demonstrated glycine increasing early & late phases of insulin secretion. In 2018, El-Hafidi et al. showed via a sucrose-fed rat model, glycine decreased the amount of oxidative stress in the liver and increased glutathione concentrations enabling greater insulin sensitivity.
Protocol: Daily dosing dependent on methionine intake → ~1:1 ratio ideal between methionine & glycine. Food sources primarily from nose-to-tail eating → bone broth, fish skin, connective meat tissue/cartilage. Obtained most easily via free-form glycine (3 - 5 g before sleep) & collagen supplementation → glycine accounts for ~33% of collagen composition.
Deficiency #7: Leucine
Mechanism: Glycine isn’t the only amino acid playing a critical role in metabolic function. Leucine is unique from other micronutrients & amino acids in that it’s not directly increasing insulin sensitivity, but more so stimulating greater insulin secretion from the pancreas. It also has a proven level of synergy with glycine in modulating the postprandial glucose response.
Evidence: When leucine & glycine were combined at 1 mmol/kg lean body mass each with 25 g glucose, glucose area under the curve decreased by 65% and insulin area response increased by 24%.
Don Layman has also detailed leucine’s impact on fat loss and improving glucose homeostasis:
“there is increasing evidence that the BCAA, and specifically leucine, have unique roles in metabolic regulation beyond the fundamental role of amino acids as substrates for synthesis of proteins…including a direct link to maintenance of glucose homeostasis by enhancing recycling of glucose via the glucose-alanine cycle and a direct link to translational regulation of muscle protein synthesis through the insulin signaling cascade.”
Protocol: Ideal intake of 3 g/meal with 10 g spread throughout the day.
Deficiency #8: Inositol
Mechanism: Our insulin signaling relies on molecules called inositol phosphoglycans (IPGs) converting insulin's signal into actual cellular actions like glucose uptake & storage. We have two main types of IPGs:
One made from myo-inositol that turns off glucose production
Another made from D-chiro-inositol that turns on glucose burning
In conditions of insulin resistance, our body loses the ability to convert myo-inositol to D-chiro-inositol disrupting both messages and creating a situation where cells can't properly respond to insulin even when it's present.
Evidence: Over the past decade, we’ve seen inositol demonstrate exceptional clinical benefits on improving glycemic regulation and more specifically treating the root cause of metabolic diseases like polycystic ovary syndrome (PCOS) & gestational diabetes. In 2019, Miñambres et al. published a meta-analysis of 20 RCTs across more than 1,200 subjects specifically focusing on the impact of inositol on glycemic response. They found improvements in fasting blood glucose, 2-hr postprandial glucose responses, insulin sensitivity (HOMA-IR), & fasting insulin levels.
Protocol: Difficult to obtain through diet. Therefore, myo-inositol supplementation preferred route → NOW Foods Inositol Powder. 4 - 6 g/day considered optimal. Absorption best prior to meals. Doses up to 18 g/day considered safe.
Deficiency #9: Betaine
Mechanism: Betaine - a modified amino acid sometimes referred to as trimethylglycine (TMG) - has a couple key roles in the glucose metabolism process. First, it serves as a methyl donor involved in the conversion of homocysteine to methionine, which regulates gene expression implicit in glucose uptake.
Betaine also upregulates fibroblast growth factor 21 (FGF21), a protein signaling molecule that enhances insulin sensitivity, promotes fatty acid oxidation, & improves glucose disposal. Animal models have suggested its absence abolishes betaine’s beneficial effects on glucose homeostasis, while conversely its supplementation enhances glucose stability.
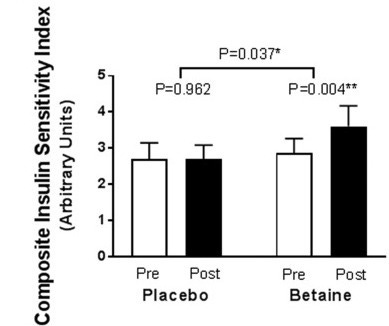
Evidence: Human evidence is limited for now with the only trial conducted to date on betaine’s impact on glycemic control. In 2018, Grizales et al. conducted a 12-week randomized, placebo-controlled trial across 27 prediabetic patients administering either 6.6 g or 10 g daily. The most notable finding was a 24% improvement of insulin sensitivity within the betaine group while no impact was observed in the placebo group.
Protocol: 4 - 6 g daily the ideal dosage split into 2 doses for metabolically healthy individuals. Up to 10 g for prediabetic/metabolically impaired/elevated liver enzymes. Total dosage obtained through a combination of grains, shellfish (oysters & mussels), select vegetables and supplementation → Nutricost Betaine Anhydrous Trimethylglycine (TMG).

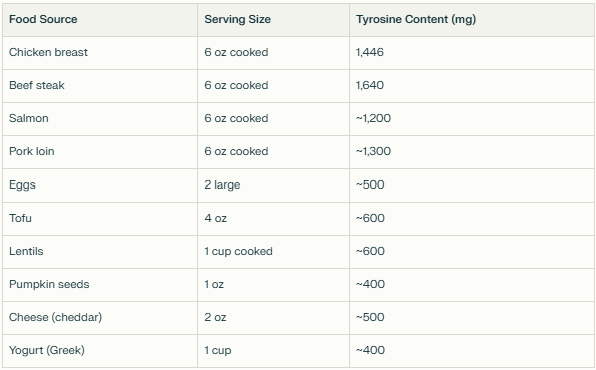
Deficiency #10: L-Tyrosine
Mechanism: Another non-essential amino acid, L-tyrosine acts as a precursor for catecholamines (like dopamine, norepinephrine, & epinephrine) and thyroid hormones (like T3 & T4).
Evidence: In 2019, Korner et al. proposed a novel postprandial mechanism where L-tyrosine is metabolized in the foregut to L-DOPA & dopamine that can eventually be taken up by pancreatic cells and suppress glucose-stimulated insulin release. If we’re deficient in L-tyrosine, the inhibitory effect gets reduced leading to greater insulin release into the blood - a vicious reinforcing loop for insulin-resistant people.
Protocol: Easily achieved via a high-protein, animal-based diet. Daily intake should equate to ~12 mg/kg BW daily (5 - 6/lb BW).
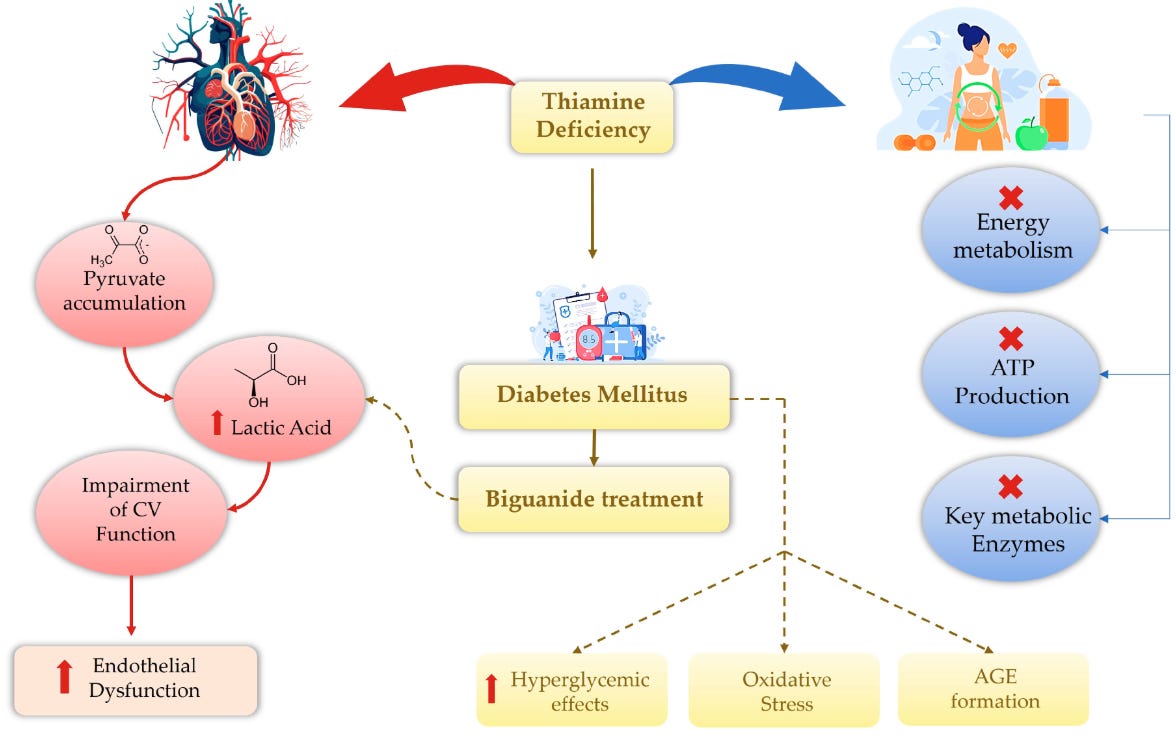
Deficiency #11: Thiamine (B1)
Mechanism: All B-vitamins in some way are implicit in a proper state of glucose homeostasis. However, Vitamin B1 (thiamine) holds the crown for its direct linkage to our ability to metabolize carbs well. Without adequate levels, key metabolic enzymes depending on it as a cofactor can’t function leading to impaired ATP generation.
Chronic thiamine deficiencies cause pyruvate to accumulate in the CV system where it's converted to lactic acid instead of entering more efficient energy-producing pathways. This lactate buildup compromises CV function: increasing blood pressure, elevating oxygen consumption, & damaging blood vessels.
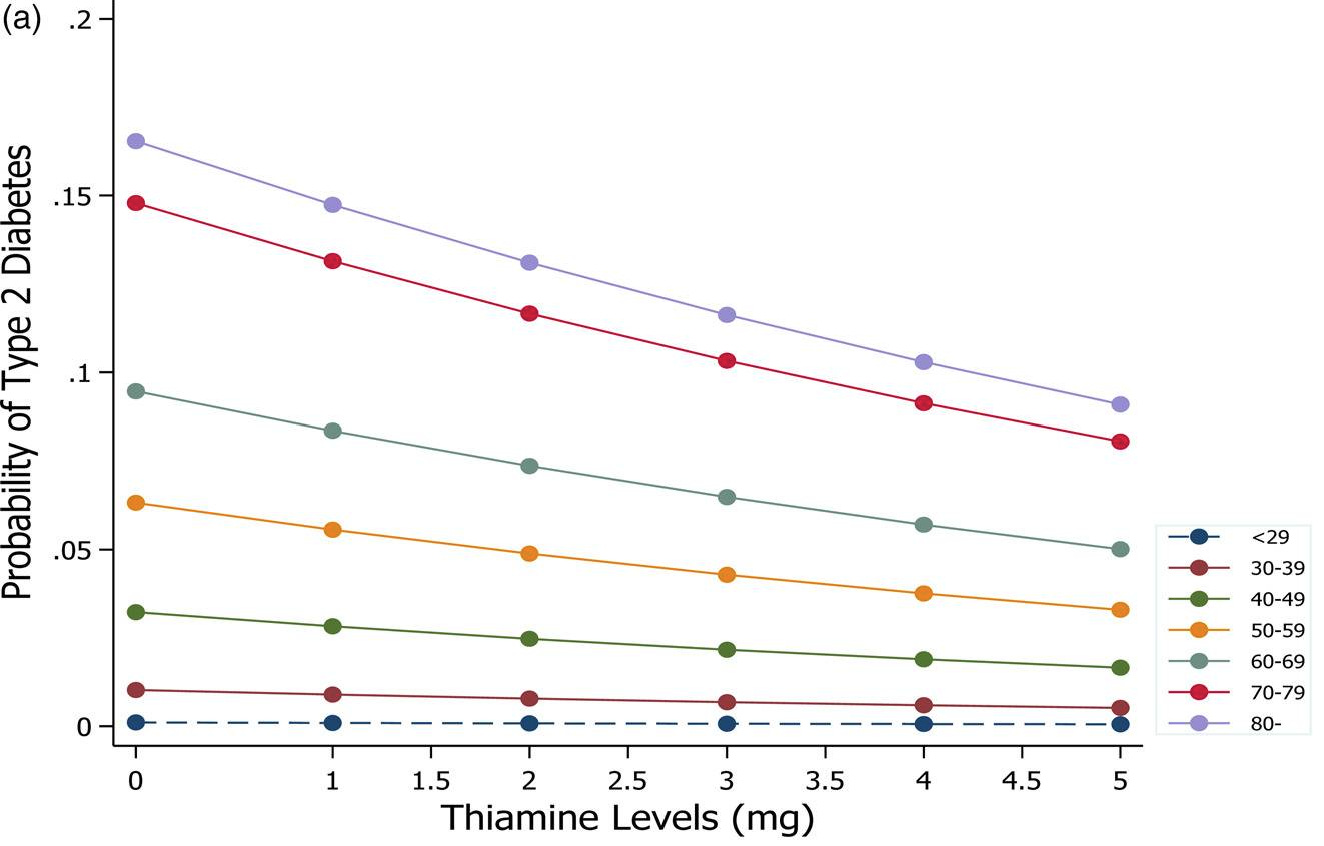
Evidence: Evidence up until this point regarding thiamine’s required role in glucose metabolism is well-established:
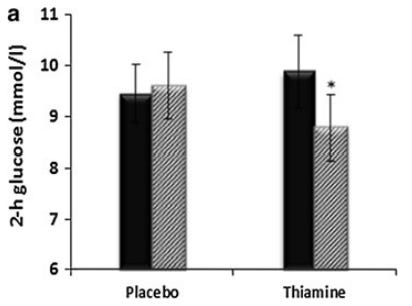
In a randomized, double-blind, cross-over design trial, Alaei Shahmiri et al. demonstrated the improvement of glycemic response. Seventeen hyperglycemic patients were administered either 100 mg thiamine or placebo 3x daily prior to meals for 6 weeks. Following the trial period, 2-hr plasma glucose improved significantly from 9.9 mmol/L at baseline to 8.8 mmol/L.
A 2021 cross-sectional study conducted by Duc et al. observed lower HbA1c & fasting blood glucose with adequate levels of thiamine consumption.
Protocol: Optimal daily intake best addressed via high vegetable intake (Brussels sprouts, squash, asparagus, okra, beets, garlic), spices (mustard, nutmeg, anise, curry, marjoram) & Thiamax supplement. Thiamax best taken with high-carb meals. Be mindful of excessive raw fish consumption as it contains thiaminase - an enzyme that rapidly breaks down thiamine in the body.
Deficiency #12: Selenium
Mechanism: Selenium supports glucose metabolism by acting as a cofactor for antioxidant selenoproteins like glutathione peroxidases reducing oxidative stress and thus mitigating insulin resistance. This protection helps preserve insulin signaling pathways while regulating glucose uptake, inflammation, & insulin sensitivity.
Evidence: In 2016, Jablonska et al. showed significant decreases in the HbA1c levels of 76 non-diabetic subjects after six weeks of 200 µg selenium supplementation daily. A more robust meta-analysis published in 2022 by Ouyang et al. covering ten RCTs demonstrated selenium supplementation significantly reduced insulin levels & insulin resistance.
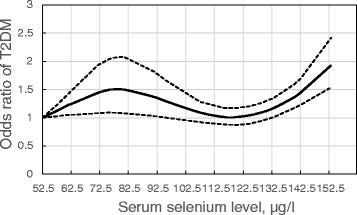
Though adequate levels are required for proper glucose metabolism, it’s best to consider selenium intake & its risk profile as a U-shaped curve (in part attributable to over consumption of kcal generally).
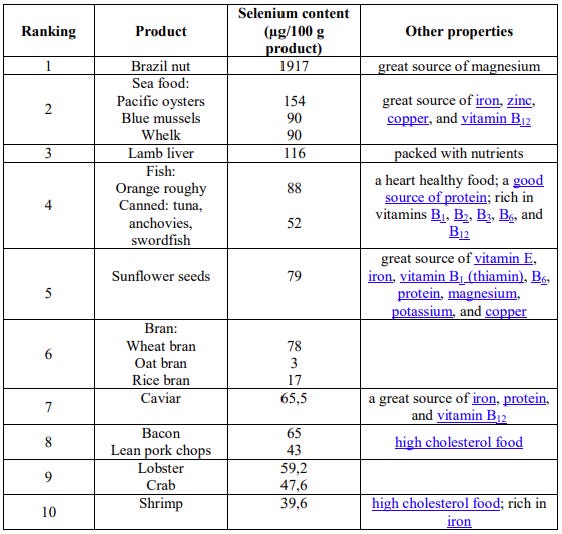
Just as a deficiency impairs insulin signaling, excess selenium supplementation has been linked to the development of insulin resistance. This is why it’s critical to avoid supplementation & shoot to obtain entirely from whole food sources.
Protocol: Optimal intake = 90 - 130 μg/day. Obtainable via bioavailable selenium sources:
Avoid selenium supplementation altogether.
Deficiency #13: Biotin (B7)
Another B-vitamin - sensing a trend? They’re all critical whether directly or indirectly involved with carbohydrate metabolism.
Mechanism: An overlooked B-vitamin, biotin functions as an essential cofactor for four carboxylase enzymes needed for glucose homeostasis. Lacking biotin, our glucokinase activity drops disrupting the balance of cells in the pancreas. Thus, increasing cells making glucagon and decreasing those that make insulin.
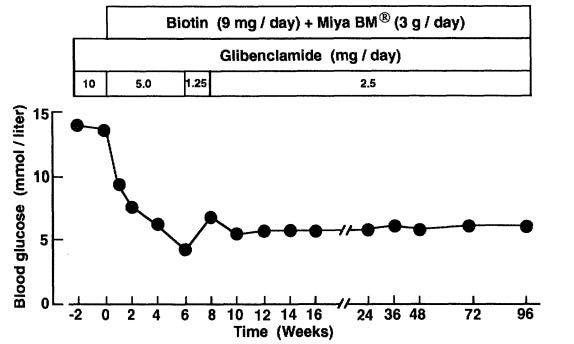
Evidence: One notable trial conducted by Maebashi et al. demonstrated a fasting blood glucose reduction following the administration of 9 mg daily.
A 2022 meta-analysis across five RCTs involving 445 subjects demonstrated that biotin supplementation over periods ranging from 4 to 12 weeks significantly reduced fasting blood glucose.
Protocol: Good rule of thumb (per Chris Masterjohn) → 150 µg for first 100 g protein & every additional 50 g protein requires an extra 35 µg biotin. Intake is especially important on a high protein diet. Avoid habitual consumption of egg whites by themselves as this can induce a deficiency via the biotin antagonist avidin.
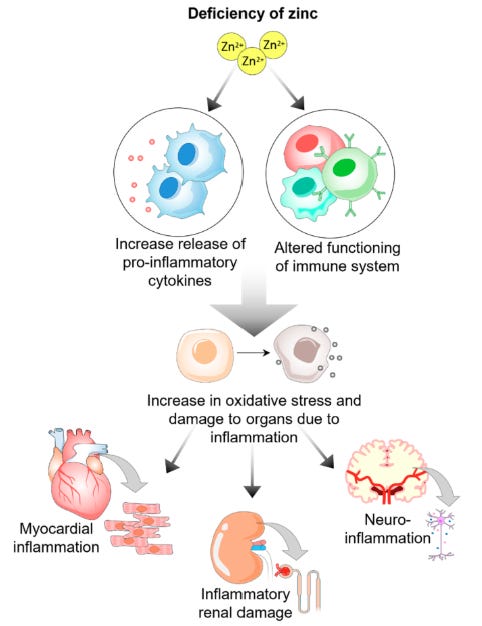
Deficiency #14: Zinc
Mechanism: Zinc transporter 8 (ZnT8) moves zinc into insulin-producing cells in the pancreas, where it helps form stable insulin crystals that can be stored and released when needed. Zinc also helps switch off enzymes that block insulin's effects. When we’re zinc deficient, these blocking enzymes become overactive and make cells much less sensitive to insulin's signals exacerbating inflammation & redox balance.
Evidence: From a clinical perspective, the evidence for zinc as a glycemic optimization tool is also robust. In a meta-analysis of 1,700 participants from 32 RCTs, zinc supplementation significantly reduced fasting & 2-hr postprandial glucose levels by an average of −14.2 mg/dL & -36.9 mg/dL, respectively. This same review showed significant decreases in HbA1c, insulin resistance, & chronic, low-grade levels of inflammation (hs-CRP).
Protocol: Zn intake should be determined in conjunction with Cu intake. Zinc to copper ratio should be ~8:1. Zn daily total shouldn’t exceed 50 mg/day. Ideally obtained through diet. Most bioavailable supplementation forms include zinc glycinate and gluconate. Avoid oxide form. Best taken on empty stomach if tolerated well.
That’s a wrap on our 14 deficiencies.
If you haven’t already, reminder to subscribe below. Every little bit makes an impact in the fight against the rampant growth of the reductionist AI/mainstream slop we're seeing. (We’re going to win.) And it’s why we’re running the Anti-Slop Summer Sale™ before we roll out more premium content.
Stay after it & until next time.
Your friend,
Phys
***Disclaimer: The information provided by BowTiedPhys is for educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment of any kind. BowTiedPhys is not a licensed medical provider. Prior to making any changes to your health protocols, consult a licensed healthcare professional. Some of the links in this post may be affiliate links - BowTiedPhys may earn a commission at no additional cost to you. This commission helps support our work and allows us to continue providing valuable content to our valued subscription members.***